Today we are going to talk about chronic phlegm in the back of your throat. To really get to the bottom of this problem, we have to think as an engineer, not as a medical professional, because when we do our research, we quickly find out that it’s all about suppressing symptoms and even classifying these conditions based on their symptoms, so that this symptom sounds like a disease. Unfortunately, they don’t go deep enough into the root causes of these issues, and they don’t let you know what the more common causes are for these symptoms.
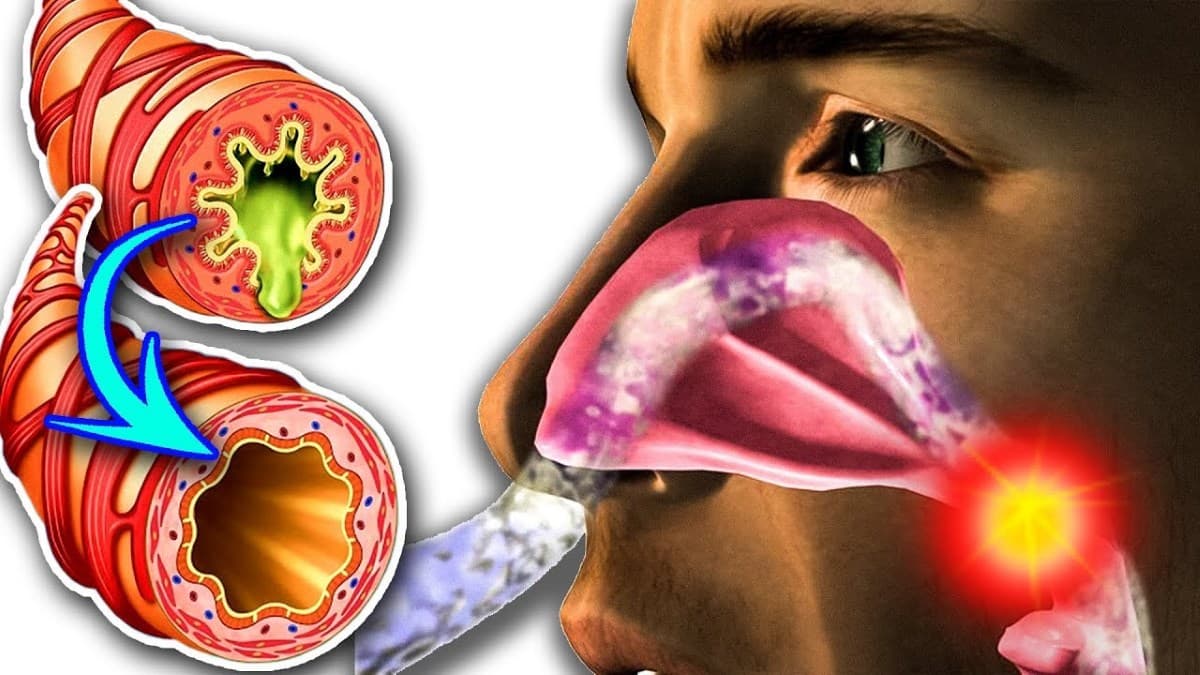
We are going to take one symptom — chronic mucus generation in the throat — and trace it back to the most likely cause. Now, with this chronic mucus production, you can have a post nasal drip, you can have chronic coughing, more at night than during the day, which I’m going to cover why that is. You can definitely have hoarseness or a scratchy throat, and you can also experience the sensation like a lump in your throat or something stuck in it or even a pain in your throat when you don’t have an infection. You’re not sure what it is.
Contents
What causes chronic phlegm?
So to take an engineering point of view, they’re going to look at a cause and effect relationship, they’re going to really look at the logic behind this problem instead of just taking this tip off the top of the iceberg symptom and then matching a medication for it to suppress it. Now we could have an allergy, we could have a virus in your sinuses producing this mucus, but the more likely cause would be something related to two other symptoms that we are going to get to the root cause.
One would be GERD, which stands for gastroesophageal reflux disease, where we have acid coming up through this valve at the top of the stomach and it’s coming up through the esophagus.
Another condition called LPR, which stands for laryngopharyngeal reflux. The basic difference between GERD and LPR (because they’re both very similar) is that the valve is not closing and so we’re getting acid that comes up with GERD into the esophagus, but with LPR we’re getting acid that comes up higher into the vocal cords, into the back of the throat.
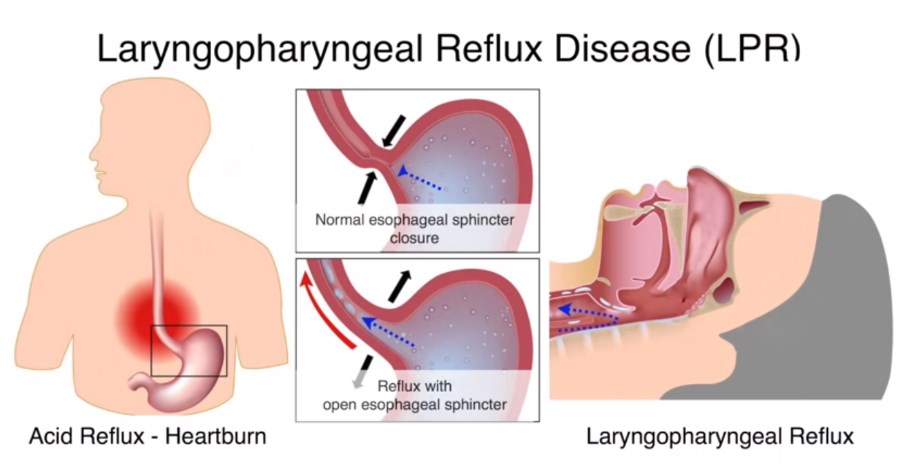
Each of these conditions is classified as a specific condition that is treated directly, usually with antacids and other medications that suppress acid in the stomach. If you have mucus in your throat, ask yourself if you have all these other symptoms associated with it. With GERD, we would have heartburn, belching or regurgitation, excess mucus, throat irritation, a lump in the throat, and difficulty breathing (because the ability to get oxygen is greatly reduced when acid rises through the throat).That is why you will have difficulty swallowing and sometimes a post-nasal cough.
It’s worse when we’re lying down at night because that valve is not closing correctly. You may also have food allergies, which we will talk more about. Another condition called LPR. We will have many of the same symptoms, but we may also have a metallic taste in your mouth and irritation of your vocal cords, like hoarseness when we are trying to talk.
A deeper look at treatments
Before we go deeper into the root cause of these issues, let us talk first about some of the treatments, which can even cause the condition or aggravate the condition even more. For example, with antacids, a big side effect would be constipation, or even acid reflux, and then we have these other medications that work a little bit differently. They’re called PPLs, protein pump inhibitors, so they basically stop the enzymes that are producing acid. They also have side effects of constipation, gas, risk for stroke, risk of getting C-DIFF, which is an infection because it’s a pathogen, palpitations, and even high blood pressure.
Then we have another side effect called hypergastronemia. What is that? That is too much gastrin, which is going to cause too much acid in our stomach. So here we are, trying to get rid of your acid by taking a solution that’s giving us more acid. That doesn’t make sense at all. Another problem with these treatments is that they will remove acid, and now we’re going to have a difficult time absorbing minerals like calcium and magnesium. That’s why now we have a problem with bones, muscles, and the list goes on. However, of course, there are other solutions too. We can get a surgery. We can tighten this valve even more, but there are some minor side effects, such as the inability to belch or burp; increased gas in our digestive system; a greater need for more antacids; and the PPIS that we just talked about. Ultimately, the optimum solution to something should not give us a bigger problem than we started out with, right?
The root cause of chronic phlegm
Let’s go deep to the most likely cause of this valve not closing, giving us GERD or LPR.
It could be an acid deficiency or low hydrochloric acid. When the acid or concentration of acid in our stomach is lower, the valve doesn’t close that properly. In fact, it can open up when the acid starts increasing, when we start digesting things like proteins, the top of the valve should close very nice and tight if everything is working correctly.
The root cause of this valve not closing is that we don’t have enough acid in the stomach, and that is the underlying reason. Because we have acid reflux, you are thinking that if we have too much acid, we need to get rid of this acid, so you’ll take an antacid or do something to reduce this, but the root cause is that we don’t have enough acid.
Why do you need hydrochloric acid?
Now, hydrochloric acid in our stomach is a very important fluid for many different things, especially within our immune system. One of the purposes of this very strong acid, which should be between one and three, is to kill pathogens.
Believe it or not, our stomach is very sterile. Nothing can live there because that acid is so strong, and this is one of the barriers that our body puts up in the immune system. Because if we can kill pathogens that come from our food into the stomach, preventing them from going down to the rest of the tract, we have a very good defense against these pathogens. However, if we have weak acid in the stomach, pathogens can escape and get into the system, creating all sorts of problems in the lower part of the digestive system. Even in the small intestine, we can get what’s called small intestinal bacterial overgrowth. That occurs because we didn’t kill the microbes at the stomach level.
Another very important purpose of this hydrochloric acid is to break down proteins. It fully breaks down proteins. So if we don’t have enough acid in our stomach, we’ll get incomplete protein digestion and start to create stress in the other parts of the digestive system, because they have to produce more enzymes and they have to do different things lower in the tract that finally throw off our whole digestion. Now, if we compound this with inflammation in the gut and we have something called leaky gut syndrome, these proteins go right into the little holes where you have leaky gut. Our immune system starts creating antibodies against these proteins, and that’s the start of autoimmune diseases. That’s the start of an allergy.
Finally, the third reason why we need this hydrochloric acid in our stomach is in our ability to absorb minerals. So, without that pH, the minerals don’t travel into the body that well. This is one of the underlying reasons why people are anemic or have mineral deficiencies—they cannot absorb minerals like calcium, magnesium, potassium, zinc, or iodine. All these minerals.
In addition, this strong pН triggers things in our pancreas to release certain enzymes as well as in our gallbladder to release bile. Without this concentrated hydrochloric acid in the stomach, being at what pH should be for the entire digestive system, starts to go downhill really fast. In addition, on top of everything else, the sensing mechanism doesn’t allow the valve to close tightly, and then the acid starts regurgitating. We may even get regurgitation of the bile up into the stomach, and both hydrochloric acid and bile can then regurgitate up through the esophagus up into our throat, irritating the back of the throat. This puts you in a constant state of mucous protection because mucus is trying to be formed an attempt to protect against the strong acid that is dissolving your tissues.
All we are talking about, is the most likely root cause of this mucous production – is chronic irritation your throat that makes us cough. Now we know that the solution is very simple because we don’t want to necessarily suppress the symptom, we want to fix the root cause, which is to increase the amount of acid in the stomach. By the way, we’re going to have to figure out, with the help of your doctor, how you can start to wean off some of these antacids. If you’re not interested, just ask them this one question: what are the long-term effects, what are the chronic effects of taking antacids over a period of time? And what’s really behind these problems, I’m sure you’ll be curious to find out what they say, but it’ll probably be something along the lines of: well, it’s just stress, genetics and as we age, most people just have these problems.
How to increase stomach acid
The way to get your stomach acid back is to take something to start building up the hydrochloric acid, and the best remedy is betaine hydrochloride. We’d want to take between three to four, to even five, six, or seven before you eat.
Now here’s the problem with certain types of people that take this. If you have an ulcer (because this condition has gone on too long), or if you have gastritis, where there’s inflammation in the stomach, and you take betaine hydrochloride, it’s going to make it worse. Because the tissues are inflamed, in which case we’re going to have to heal the lining of your stomach first, which could take anywhere between two to three months. Before you start adding more acid to the system, you need to understand the mechanism here. You need to know that, ultimately, you want to acidify the stomach and get it back to normal. There are other things we need to do because the foods that we’re eating are probably not helping you.
And the biggest offender in this problem is grains. Now what’s wild is that if we look this up, they will tell us to consume grains to improve our acid reflux, but in reality we’re going to find that makes a lot worse. There are a lot of things in grains that are inflammatory. That creates sensitivity, allergies, autoimmune conditions, and even lowers our immune system and dumps a lot of omega-6 fatty acids into the system. A typical grain has like 20 or more times. the omega-6 than it does for the omega-3, which are anti-inflammatory, so we’re basically dumping a lot of inflammation in our system when we consume grains and consume animal products that were fed a lot of heavy grains versus grass-fed, brass-finished animal products. Always remember to think outside the box and see if we can start to sort out our own diet and what we need to change.
It’s also essential to do intermittent fasting and not follow the rule of just having five or six small meals throughout the day. No, we don’t want to do that. We want to do intermittent fasting because the more that you do intermittent fasting, when you fast for a period of time, at least 16–17–18 hours, by skipping our breakfast. We can give our digestive system a chance to rest, heal, and recover because it’s not constantly being triggered by foods. Another big cause of this entire problem is low stomach acids and a lack of bile salts, which can inhibit our ability to digest fats on a vegan diet.
When someone is a vegan, many times they consume a lot of grains and a lot of foods that tear up their digestive system, and they don’t consume a lot of animal fats, and because they’re not consuming a lot of animal proteins, they might not have the triggering of this hydrochloric acid. The combination of all these inflammatory foods and the missing nutrients that are in a vegan diet can create havoc on our digestive system. That being said, there is a correct way to do a vegan diet, but dint forget to stay away of all the kinds of artificial meats, soy protein isolates, grains, sugar, etc.



I used to suffer with this issue BIG-TIME. The symptoms I experienced (lump in throat, excess mucus, and regurgitation…god the regurgitation was awful) were so bad that they affected my sleep greatly. I would wake up after a “night’s rest” feeling like I had slept for 20, 30 minutes tops. It honestly made life very difficult for me, and I was often at my wits end for what to do besides using antacids or PPI. I mean, for god sakes, I was 21 at the time, why does a 21 year old need antacids? But in a way, having this condition may have helped me take greater control of my health. At some point I was so fed up that I actually did some research into the root causes (like Dr. Berg) suggested and found that it could be diet-related, or it could be due to lack of stomach acid…etc. I guess I was a lot more naive then so it took me much longer to come to the conclusion that it was a problem I could fix through lifestyle modification rather than strictly medication.
What I found, for me personally, was that food definitely had an impact. I used to consume a lot of protein powder after working out, and it certainly wasn’t high quality. I cut that out, along with dairy. That provided a slight improvement. I then found out about the Betaine-HCL (Not sure if it was through Dr. Berg, can’t remember) and I bought that as well. Started using that and again, after two weeks or so, saw more minor improvements. Well, that gave me a lot of hope. I tried to make my diet as clean as possible, just for one month, to see how well I could benefit. In addition, I began consuming a LOT of fermented foods, specifically kefir and sauerkraut. That seemed to have a HUGE benefit. Lastly, I also considered the fact that my gut lining was probably damaged due to terrible diet, medications, you name it. So I was taking “L-glutamine” for a good period of time in order to remedy that. That felt like a much slower change over time, but I do think it had positive effects. I also took Zinc Carnosine for a period of time. The combo of these pretty much gave me my life back. I’ll summarize it below:
-Cutting out certain foods (for me, dairy/protein powders)
-Using Betaine-HCL with meals to improve stomach acid
-Clean up diet (kinda goes along with the first one)
-Consume fermented foods (Kefir, sauerkraut, etc)
-L-glutamine (Positive effects on gut lining and repair)
-Zinc Carnosine (for stomach lining)
Hope that helps. I know I wrote a wall of text here but this issue affected my life for so long that I want to assist anyone suffering with this condition in any way I can.