
There is some really interesting information relating to an autoimmune disease. If you have an autoimmune condition, this article is going to enlighten you about a protocol that you may or may not know about.
Contents
The Coimbra protocol
This information is about the Coimbra Protocol by Dr. Coimbra. He’s a Brazilian neurologist. This is what he said. All or nearly all patients with autoimmune disease have increased resistance to the effects of vitamin D (learn more about the benefits of Vitamin D). Today, there are thousands of scientific peer-reviewed studies linking the vitamin D levels to autoimmune diseases. In other words, if you have an autoimmune disease, chances are you’re low in vitamin D.
However, Dr. Coimbra took it one step further and found out that there’s not just a deficiency of vitamin D, there’s a resistance to vitamin D. He noticed that in order to raise the vitamin D levels in these patients with autoimmune diseases, it requires much higher doses than in the average population. For example, if we’re going to maintain vitamin D levels in a healthy person, we’d probably want to use 10,000 IUs. This is also based on quite a few credible sources like Dr. Michael Hillock, who’s the authority on vitamin D, discusses taking 10 000 IUs of vitamin D without any chance of toxicity versus the medical health care system, in general, recommending only 600 IUs of vitamin D per day. When we give a patient who has an autoimmune disease 10 000 IUs of vitamin D3, we may notice only a slight partial improvement. Therefore, this topic is very important, especially since 50 million people in the US have autoimmune conditions.
Vitamin D explained
Vitamin D is not really a vitamin; it’s a hormone. It is chemically very similar to steroid hormones. That’s why it creates some very similar effects to cortisol. It’s a very powerful anti-inflammatory. It helps to calm down an overactive immune system. One of its amazing functions is its ability to act as an immune regulator. So it regulates the immune system. If the immune system is attacking itself, that’s out of control, and that’s what an autoimmune condition is, is, whether it’s lupus, rheumatoid arthritis Сrohn’s, Hashimoto’s, or whatever or something else, the common thread in all these diseases is inflammation and low vitamin D levels.
A look at vitamin C and scurvy
My question is, since there is so much data on this relationship between low vitamin D levels and autoimmune disease, why don’t doctors recommend this more often? Well, I’m going to refer us to vitamin C in scurvy. In 1595, the world faced a serious problem with selling ships. Sellers were dying. There was no cause, no cure.
Then, in 1601, several years later, Captain James Lancaster decided to give one teaspoon of lemon juice daily to a certain group of sailors, and all of those sailors did not die. But a good percentage of those who didn’t take it died, about 40. It was known back in 1595 that something in lemon juice prevented scurvy, which is a very serious and deadly condition.
Then, in 1753, James Lind published a study on scurvy, and he concluded a sudden, invisible effect for scurvy when you fed these sailors oranges and lemons. Now you would think this would be disseminated, people would accept it, and the medical profession would welcome this great information, right? Not quite.
In fact, even James Lib himself said that it wasn’t the vitamin C primarily. That was a secondary effect. He said that scurvy was caused by moisture, and we had to keep these sailors in a dry environment. In 1795, Gilbert Bain persuaded the royal navy to give lemon juice to sailors. But it took 70 years. Later, in 1865, before the intake of a lemon was finally recommended to prevent scurvy, but even that didn’t convince everyone. So it was soon discredited for about 60 more years until they actually discovered vitamin С.
Thus, vitamin C was discovered in 1932. Even during the Civil War, which lasted from 1861 through 1865, 7,000 Union troops died of scurvy. Another 45, 000 troops died directly of scurvy and dysentery, which is an infection that affects the digestive system as well as diarrhea. In 1849, when they had the California gold rush, 10,000 people died, and then during the Irish famine with the potato crops in the 1840s, over a million people died of scurvy. So, it takes a long time for the medical profession to adopt new ideas. With this whole vitamin D deficiency linked to autoimmune disease, it could probably take another 150 to 200 years before they really fully accept this. In the meantime, there are people who will adhere to this conventional wisdom.
Vitamin D for autoimmune conditionals
Even now, there are so many side effects because the treatment for autoimmune disease is mainly steroids. Steroids have some massive side effects, but vitamin D does not. Vitamin D works very similar to the steroid cortisol, but without the side effect. Now, when we’re using higher doses of vitamin D, potentially we could get hypercalcemia, and the biggest problem with that is kidney stones. However, when we talked about the protocol, Dr. Coimbra came up with a solution for this potential side effect. We have to realize that it takes high doses of vitamin D over months to create hypercalcemia.
Thus, vitamin D is not really a vitamin. It is a hormone; it acts like a steroid, but it doesn’t have the side effects. But it is different than most hormones because hormones have a very specific target tissue that they go after. For example, the hormones testosterone, cortisol, other hormones, or even estrogen, go after very specific tissues, but with vitamin D, which I don’t even like to call it a vitamin, has receptors, targets are in every cell in the body. We have 229 different genes that are directly influenced by vitamin D and are associated with 25,000 different functions. It is the most important vitamin simply because it does so many different things, and so many people are deficient in this vitamin.
Vitamin D resistance
There’s something even more interesting. Do you remember we mentioned the term “resistance”? You’re resistant to vitamin D. One big way someone is resistant to vitamin D is a problem with the vitamin D receptor. That condition is called vitamin D polymorphism, which is an alteration in the receptor for vitamin D. In other words, if someone has this defect in the receptor, they’re going to be very resistant to absorbing vitamin D. They’re going to have to take a lot more than a person who doesn’t have this problem.
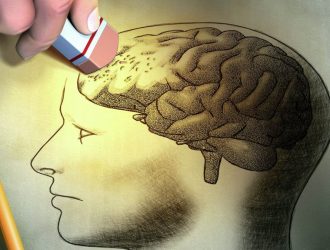
To make this simple to understand, we can look at a polymorphism as a mutation, which is some change in the genetics. We can develop a polymorphic change or a mutation in the gene through either having it inherited from our parents or developing it in this life from the environment spontaneously. The drug severe overwhelming stress, which could explain why so many people develop autoimmune diseases after a severe loss of a loved one, a severe stress event, or a trauma.
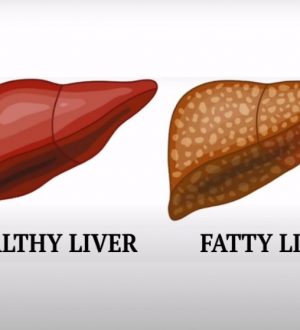
Thus, the more resistant we are to vitamin D, the more prone we are to autoimmune diseases such as type 1 and type 2, cancer, bone loss, and even hives. Not to mention all the other factors that cause resistance, such as skin color—the darker the skin, the harder it is to absorb vitamin D because the pigment melanin blocks the ultraviolet light that is needed to form vitamin D through the skin. Then we have the metabolic syndrome or insulin resistance factor, which can block your ability to absorb vitamin D.
Obesity. The more fat we have, the less we’re going to absorb vitamin D. Then there’s age. The older we are, the less we’re going to absorb vitamin D. In addition, of course, we have the diet from which it’s even harder to get vitamin D because there are not many foods that will give it to you unless you’re consuming fatty fish, salmon, cod liver oil, and things like that. And on top of all that, we just don’t get much sun exposure. People stay inside all the time; they don’t get out there to get that sun. Not to mention, if they do, they put a bunch of sun lotion on their bodies to prevent the UV radiation.
How to do the Coimbra protocol
This is all very interesting, but what is the protocol? That’s what we are going to cover right now.
Now, when doing this protocol, it would be important to find a doctor that can work with you. We’re going to do a test for vitamin D before we start, but we’re not going to determine the dosage of vitamin D by our vitamin D levels. Why? Because we have this resistance, remember? So we’re going to determine the dosage by measuring something else, and that’s called the parathyroid hormone, or what’s called parathormone. When we take vitamin D, it suppresses the parathyroid hormone. So the more vitamin D you take that gets absorbed, the less parathyroid hormone you’re going to have. Thus, the goal of this whole protocol is to drop your parathyroid hormone into the lower level of the normal range.
If our parathyroid hormone is high, it usually means that we’re low in vitamin D, or it’s being resistant it’s just not going in. Now as far as the amount of vitamin D that someone is going to take, it could range anywhere between 40 000 to 200 000 IUs per day (depending on a couple factors), one being your body weight as well as the parathyroid hormone. This is why, typically, the rough formula for how much vitamin D we’re going to start with would be a thousand IUs per kilogram of body weight. Now, to minimize the main side effect of this protocol, which is kidney stones, what he recommends is avoiding calcium as a supplement, as in hard water, as in nuts. This is happening because nuts have a good amount of calcium like in tofu or other soy products, which do have calcium, and anything related to dairy products such as milk, cheese, yogurt, etc.
Finally, yet importantly, is that we’ll drink about two and a half liters of fluid a day. So you can have the benefits of vitamin D without the one big side effect: kidney stones. It usually takes about two months to see the changes in the blood consistently, but then over the course of two years we’d be checking the parathyroid about four times, and making adjustments throughout. Then, within two years, once you’re stabilized, then we’ll be on a maintenance type program. Again, this might sound complex or difficult, but from the general point of view, if we have an autoimmune disease and we want to weigh out the risks and benefits of being on prednisone long-term versus doing this, it makes no sense.





I had stage 4 cancer and beat it. I was fairly healthy based on standard measures but not really (obviously). I changed a lot of things. I increased my vit D to 20k daily. I also take triple vit K along with it. After 5 years of this plus my regular multiple plus 1tbl daily of cod liver oil, I show no signs of sickness or toxicity from the D. And even though I used to get kidney stones pre cancer, on my new routine I have had no problems.